Cancer
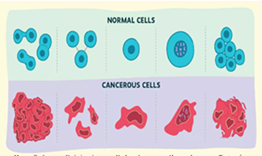
Cancer refers to a group of diseases in which body cells grow and multiply in an abnormal and uncontrolled manner. These cells can invade surrounding tissues, spread to distant organs (metastasis), and may result in death if the condition is not detected and treated at an early stage. Cancer can develop in any part of the body and may originate from any type of cell.
Major categories of cancer
1. Carcinomas: Carcinomas develop from epithelial cells that form the lining of internal organs and the surface of the skin. They are the most common type of cancer. Common examples include cancers of the mouth, oesophagus, intestine, uterus, and skin.
2. Sarcomas: Sarcomas originate from connective or mesodermal tissues of the body. These include tissues such as bone, cartilage, fat, and fibrous tissue. Examples are cancers of bone, fat, cartilage, and fibrous tissue.
3. Cancers of the blood and immune system: These cancers arise from cells of the bone marrow and the immune system. They include leukaemia, lymphoma, and multiple myeloma.
Problem statement
Cancer is a major public health problem and one of the leading causes of death worldwide. In 2018, about 18 million new cancer cases and 9.6 million deaths were reported globally, and nearly 70% of these deaths occurred in developing countries. Due to population growth, aging, and lifestyle changes, the number of cancer cases is increasing every year. In 2022, around 20 million new cancer cases and nearly 10 million deaths were reported worldwide. If the current trend continues, global cancer cases may rise to 35 million by 2050.
In India, the cancer burden is also increasing. According to the World Health Organization (WHO) and the International Agency for Research on Cancer (IARC), India reported about 1.41 million new cancer cases and around 9.1 lakh deaths in 2022. India ranks third in the world for cancer cases, after China and the United States. By 2024, more than 1.53 million new cancer cases were recorded in the country.
In Nepal, cancer is an increasing public health concern. Data from the Global Cancer Observatory (2022) show that Nepal had about 22,000 new cancer cases and nearly 14,700 cancer-related deaths. Lung cancer is the most common cancer among men, while breast and cervical cancers are the most common among women.
Causes of cancer
As with other chronic diseases, cancer has a multifactorial aetiology.
1. Environmental factors (80 to 90 per cent of all human cancers)
(a) Tobacco: Tobacco (e.g. smoking, chewing) is the major cause of cancers of the lung, larynx, mouth, pharynx, oesophagus, bladder, pancreas and probably kidney. Cigarette smoking is now responsible for more than one million premature deaths each year.
(b) Alcohol: Excessive intake of alcoholic beverages is associated with oesophageal and liver cancer. Alcohol contributes to about 3 per cent of all cancer deaths.
(c) Dietary factors: Smoked fish is related to stomach cancer; a high-fat diet to breast cancer. Other dietary factors include food additives and contaminants.
(d) Occupational exposures: Exposure to benzene, arsenic, cadmium and asbestos.
(e) Viruses: Hepatitis B and C viruses are causally related to hepatocellular carcinoma.
(f) Customs, habits and lifestyles: Familiar examples are the demonstrated association between smoking and lung cancer, tobacco and betel chewing and oral cancer, etc.
(g) Others: Sunlight, radiation, air and water pollution, medications (e.g. oestrogen) and pesticides.
2. Genetic factors
Genetic influences have long been suspected. For example, retinoblastoma occurs in children of the same parent. Mongols are more likely to develop cancer (leukaemia) than normal children. However, genetic factors are less conspicuous and more difficult to identify. There is probably a complex interrelationship between hereditary susceptibility and environmental carcinogenic stimuli in the causation of a number of cancers.
Cancer control
Cancer control includes a group of activities based on current medical knowledge. Its aim is to prevent cancer, detect cancer early, provide proper treatment, and offer rehabilitation and after-care.
The main goals of cancer control are to:
- Reduce the number of new cancer cases
- Increase cure and survival rates
- Reduce disability and suffering caused by cancer
Cancer control mainly focuses on primary prevention and secondary prevention. It is estimated that at least one-third of all cancers can be prevented by avoiding risk factors and adopting healthy lifestyles.
1. Primary prevention
Primary prevention focuses on preventing the development of cancer by addressing causative factors and encouraging healthy behaviors. Key measures include:
- Control of tobacco and alcohol use: Reducing tobacco use and limiting alcohol intake can significantly lower cancer risk. Tobacco control alone could prevent over a million cases of cancer annually.
- Personal hygiene: Maintaining proper hygiene can help prevent cancers such as cervical cancer.
- Radiation exposure: Minimizing unnecessary exposure to radiation, including medical imaging, while ensuring diagnostic benefits.
- Occupational safety: Protecting workers from industrial carcinogens through proper safety measures and regulations.
- Immunization: Vaccination against hepatitis B reduces the risk of liver cancer, while HPV vaccination helps prevent cervical cancer.
- Safe foods, drugs, and cosmetics: Ensuring products are free from carcinogenic substances.
- Air pollution control: Reducing exposure to environmental pollutants that may contribute to cancer development.
- Treatment of precancerous lesions: Early detection and management of lesions, including cervical tears, intestinal polyps, warts, chronic gastritis, chronic cervicitis, and adenomata.
- Legislation: Enforcing laws to limit exposure to known carcinogens such as tobacco, alcohol, and industrial chemicals.
- Cancer education: Raising awareness about early warning signs (e.g., breast lumps, changes in moles, persistent cough, abnormal bleeding, non-healing sores, unexplained weight loss) to encourage early diagnosis and timely treatment.
Note: While primary prevention has great potential, it requires significant resources and ongoing research to achieve maximum effectiveness.
2. Secondary prevention
Secondary prevention emphasizes early detection and timely management of cancer to improve outcomes. Key measures include:
- Cancer registration: Collecting accurate data through hospital-based and population-based cancer registries is essential for planning and monitoring control programs.
- Screening programs: Detecting cancer at pre-invasive or pre-malignant stages can improve prognosis. Effective screening exists for cancers such as cervical, breast, and oral cancers.
- Treatment and after-care: Patients diagnosed early should have access to appropriate treatments, including surgery, radiotherapy, chemotherapy, or a combination. For advanced cases, palliative care and pain management are crucial, as freedom from cancer-related pain is now recognized as a basic patient right.
Cancer screening
Early detection and prompt treatment of cancer and precancerous conditions offer the best protection for individuals and communities. Cancer screening, defined as the “search for unrecognized malignancy using rapid tests,” is now a major focus. Screening is effective because many cancers are preceded by premalignant lesions, most begin as localized tumors that are highly curable if detected early, and about 75% of cancers occur in accessible body sites.
Methods of cancer screening
1. Mass screening by comprehensive cancer detection
This method involves a rapid clinical examination of one or more body sites by a physician. It is applied to the general population to detect cancer at an early stage.
2. Mass screening at single sites
Screening is focused on specific organs or body sites using appropriate tests. Common examples include:
- Cervical cancer: Pap smear or Visual Inspection with 5% Acetic Acid (VIA)
- Breast cancer: Breast self-examination (BSE), clinical breast examination (CBE), and mammography
- Lung cancer: Chest X-ray and sputum cytology (mainly for high-risk individuals).
3. Selective screening
Selective screening targets high-risk groups to use resources efficiently. Examples include:
- Women aged 35 years and above from lower socio-economic groups for cervical cancer
- Chronic smokers for lung cancer.
1. Screening for cancer of the cervix
Cervical cancer screening is an important preventive practice that can detect cancer in situ, the early, non-invasive stage of cervical cancer confined to the cervical lining. The Pap smear test is the primary method for identifying these early lesions. Women are advised to begin screening at the onset of sexual activity and repeat it every three years, along with regular pelvic examinations. Population-based screening programs have successfully reduced cervical cancer incidence and mortality in many countries.
Since Pap smear screening requires laboratory facilities, trained personnel, and equipment, Visual Inspection with 5% Acetic Acid (VIA) is often used as a cost-effective alternative in low-resource settings. VIA is easy to perform, sensitive, and can be conducted by trained health workers. Pap smear and biopsy remain essential for confirming abnormal findings and guiding further management, especially when cancer in situ or invasive lesions are suspected.
2. Screening for breast cancer
Screening reduces mortality by detecting breast cancer at an early and treatable stage. The main methods include:
a. Breast Self-Examination (BSE): Women should perform regular BSE, as many breast cancers are first noticed by the women themselves rather than during routine physician exams. While its effect on mortality is not fully quantified, BSE is a useful tool for early detection and remains the most feasible method for wide coverage in many developing countries.
b. Clinical Breast Examination (CBE): CBE involves palpation of the breast by a physician or trained health worker to detect lumps or abnormalities. Sensitivity may be reduced in women with large or fatty breasts.
c. Thermography: Thermography detects temperature differences in breast tissue without radiation exposure. However, it is not sensitive or reliable and is generally not recommended for screening.
d. Mammography: Mammography is the most sensitive and specific method for detecting small or non-palpable tumors. Limitations include:
- Radiation exposure: Each mammogram delivers about 500 milliroentgen, compared to 30- 40 milliroentgen from a chest X-ray. Cumulative exposure may pose a risk.
- Technical requirements: Requires specialized equipment and trained radiologists, which limits large-scale use in low-resource settings.
- False positives: Biopsies of suspicious lesions may produce 5–10 false positives per true cancer, leading to anxiety and unnecessary procedures.Bottom of Form
3. Screening for lung cancer
Currently, only two methods are available for lung cancer screening:
- Chest radiography (x-ray)
- Sputum cytology
Mass radiograph at six-month intervals have been suggested for early detection. However, evidence does not show a clear reduction in lung cancer mortality, so routine mass radiograph screening is not recommended. Similarly, sputum cytology, whether alone or combined with chest X-rays, has not been proven effective in lowering mortality. Overall, lung cancer does not meet the criteria for effective population-based screening, and routine screening is therefore not recommended.
Epidemiology of selected cancers
1. Oral cancer
Oral cancer remains a significant global health concern, especially in Asia, where tobacco use, smokeless tobacco habits, and alcohol consumption are widespread. According to the most recent data from GLOBOCAN and the World Cancer Research Fund, there were approximately 389,846 new cases of mouth and oral cavity cancer worldwide in 2022, with a global age-standardized incidence of about 4.0 per 100,000 populations. South Asia bears a particularly high burden, reporting over 92,000 new cases in 2021 and approximately 97,154 deaths, representing one of the highest mortality rates globally. In Nepal, oral cancer continues to be a pressing public health issue, with around 959 new cases of lip and oral cavity cancer estimated in 2022, making it one of the more frequently diagnosed cancers in the country.
Epidemiological features
- Tobacco use: Around 90% of oral cancers in South-East Asia are linked to tobacco, whether smoked or chewed. Risk is especially high for individuals who keep tobacco in the mouth overnight.
- Alcohol: Excessive alcohol use increases the risk and has a synergistic effect with tobacco.
- Precancerous stage: Lesions such as leukoplakia and erythroplakia can precede invasive cancer for up to 15 years. Early detection can lead to regression or successful treatment.
- High-risk groups: Tobacco chewers and smokers, bidi users, betel quid chewers, and individuals sleeping with tobacco in the mouth.
- Cultural practices: Indigenous tobacco forms like bidi, chilum, hookah, and khaini are common, especially among lower socio-economic groups.
Prevention
- Primary prevention: Focuses on eliminating tobacco through education, awareness campaigns, and legislative action.
- Secondary prevention: Oral cancer is easily detectable visually. Community health workers can identify precancerous lesions early. Surgery and radiotherapy are primary treatments.
2. Cervical cancer
Cervical cancer is the second most common cancer among women globally, with approximately 527,624 new cases and 265,653 deaths each year. Developing countries account for almost 88% of cases. In Nepal, the crude incidence is 24.2 per 100,000 women, with around 3,504 new cases and 1,872 deaths annually.
Cervical cancer remains a major global health challenge for women. According to the latest estimates, an estimated 662,301 new cases and about 348,874 deaths from cervical cancer occurred worldwide in 2022, making it the fourth most common cancer among women globally, with the vast majority of cases and deaths occurring in low‑ and middle‑income countries.
In Nepal, cervical cancer continues to be a leading cancer among women. Recent estimates indicate that around 2,244 new cases and 1,493 deaths occur annually, with a crude incidence rate of approximately 16.4 per 100,000 women, which is significantly higher than the World Health Organization’s elimination target of 4 per 100,000.
These figures reflect persistent risk factors such as persistent infection with high‑risk human papillomavirus (HPV), limited access to screening, and low awareness, which contribute to late diagnosis and high mortality in Nepal and other low‑resource settings.
Risk factors
- Age: Most cases occur between 25 and 45 years.
- Genital warts: Presence of warts indicates increased risk, linked to sexually transmitted infections.
- Sexual behaviour: Higher incidence among widowed, divorced, or women with multiple sexual partners; rare among virgins.
- Early marriage and childbearing: Early sexual activity and multiple pregnancies increase risk.
- Oral contraceptive pills: Long-term use, especially high-estrogen pills, may increase risk.
- Socio-economic status: Limited access to health care and poor genital hygiene contribute to higher incidence among lower-income women.
Prevention and control
- Primary prevention: Improved hygiene, reproductive health, family planning, and safe sexual practices reduce risk. Developed countries show decreased incidence due to better health services.
- Secondary prevention: Screening is most effective. Pap smears and HPV testing detect precancerous or early-stage lesions. Treatments include radical surgery and radiotherapy.
- Survival rate:
- Carcinoma in situ: ~100% 5-year survival
- Localized invasive disease: ~79%
- Regional invasive disease: ~45%
Breast cancer
Breast cancer is the most frequently diagnosed cancer among women worldwide. In 2022, there were an estimated 2.3 million new cases of female breast cancer globally, making it the most common cancer in women in 157 out of 185 countriesand accounting for about1 in 4 cancer cases in women. It is also theleading cause of cancer death in women, with approximately670 000 deaths worldwide in the same year. On average, 1 in 20 women worldwide will be diagnosed with breast cancer in her lifetime. If current trends continue, by 2050 the global burden is projected to rise to about 3.2 million new cases and 1.1 million deaths per year due to factors such as population growth, aging, and changing exposure to risk factors.
Risk factors
- Age: Risk increases sharply between 35 and 50 years.
- Family history: Women with a first-degree relative diagnosed before menopause are at higher risk.
- Parity: Early first full-term pregnancy is protective; delayed first pregnancy increases risk. Nulliparous women have similar risk to those who never gave birth.
- Menstrual history: Early menarche and late menopause increase risk; surgically induced menopause reduces risk.
- Hormonal factors: Elevated estrogen and progesterone levels increase susceptibility.
- Prior breast biopsy: History of benign breast disease increases risk.
- Diet and obesity: High-fat diets and obesity are associated with higher risk.
- Socio-economic status: Higher incidence among women in wealthier groups, possibly due to delayed childbirth.
- Other factors: Radiation exposure and prolonged oral contraceptive use before first pregnancy slightly increase risk.
Prevention
- Primary prevention: Reduce modifiable risk factors, promote awareness, encourage exercise, healthy diet, and maintain ideal body weight.
- Secondary prevention: Early detection through screening improves outcomes. Regular follow-up is essential to detect recurrence or new tumors early. Early treatment generally has a better prognosis than delayed intervention.
4. Lung cancer
Lung cancer is the leading cause of cancer-related deaths worldwide, with the highest mortality rates among both men and women, and smoking remains the leading cause, responsible for approximately 85% of all cases. Although recognized in medical literature in the late 19th and early 20th centuries when it was still rare, lung cancer incidence rose rapidly during the 20th century, becoming a major public health problem in Western men by the 1930s as cigarette smoking became widespread and later increasing in women as smoking patterns shifted from the 1960s onward.
Epidemiological features
- Age and sex: About one-third of lung cancer deaths occur before 65 years. Incidence is rising faster in females than males in industrialized countries.
- Smoking: Strong causal link established. Risk depends on number of cigarettes, age at initiation, duration, inhalation depth, and nicotine/tar content. Passive smoking also increases risk. About 90% of lung cancer deaths in countries with widespread smoking are attributable to tobacco.
- Other factors: Air pollution, radioactive exposure, and occupational exposure to asbestos, arsenic, chromates, nickel dust, and polycyclic aromatic hydrocarbons. Smoking combined with asbestos exposure significantly increases risk.
Prevention
- Primary prevention: Focus on controlling tobacco use. Strategies include mass education, legislative restrictions, taxation, health warnings, and smoking cessation programs.
- Secondary prevention: Early detection using chest X-ray or sputum cytology is possible but not widely effective. Mass screening is not recommended due to high cost and limited impact.
- Treatment: Poor outcomes; median survival is 2–3 months untreated, 10–14 months with chemotherapy. Palliative care is important for advanced disease.
5. Stomach (Gastric) cancer
Stomach cancer remains one of the most common cancers worldwide. In 2022, there were an estimated 968,784 new cases of stomach cancer globally, making it the fifth most common cancer by incidence. An estimated 660,175 deaths from stomach cancer occurred worldwide in 2022. The disease shows wide geographical variation, with the highest numbers of cases and deaths in Eastern Asia, especially China, followed by other Asian countries and parts of Europe.
Age-standardized incidence and mortality rates vary significantly across regions, with the highest rates in Eastern Asia.
Risk factors
- Dietary habits, high salt, cured or preserved foods
- Low intake of fresh fruits and vegetables
- Infection with Helicobacter pylori
- Decline in industrialized countries attributed to better food preservation and nutrition
Clinical features
- Non-specific symptoms like weight loss, fatigue, indigestion
- Diagnosis by barium X-ray or endoscopy with biopsy
Treatment
- Surgical removal of the tumor, sometimes with chemotherapy
- Prognosis poor: overall 5-year survival <20%, but 60% survive if detected early
Screening
- Japan uses photofluoroscopy for mass screening; mortality decline observed, though the effect of diet and early treatment is also influential.
References
- Park, K. (2019). Park’s Textbook of Preventive and Social Medicine (25th ed.). Jabalpur, India: Banarsidas Bhanot Publishers.
- American Cancer Society. (n.d.). Global Cancer Facts & Figures. Retrieved January 12, 2026, from https://www.cancer.org
- International Agency for Research on Cancer (IARC). (2022). Nepal: GLOBOCAN 2022 Fact Sheet. World Health Organization. Retrieved January 12, 2026, from https://www.iarc.who.int
- International Agency for Research on Cancer (IARC). (2022). India: GLOBOCAN 2022 Fact Sheet. World Health Organization. Retrieved January 12, 2026, from https://www.iarc.who.int
- World Cancer Research Fund International. (n.d.). Mouth and oral cancer statistics. Retrieved January 15, 2026, from https://www.wcrf.org/preventing-cancer/cancer-statistics/mouth-and-oral-cancer-statistics/
- Kantipur Dental College. (n.d.). Publications on oral health and cancer. Retrieved January 15, 2026, from https://www.kantipurdental.edu.np/uploads/publications/publications-1748154884.pdf
- World Health Organization (WHO). (n.d.). Cervical cancer – Fact sheet. Retrieved January 15, 2026, from https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
- International Journal of Gynecological Cancer. (2025). Relevant gynecological cancer research article. Retrieved January 15, 2026, from https://www.sciencedirect.com/journal/international-journal-of-gynecological-cancer
- World Health Organization (WHO). (n.d.). Breast cancer – Fact sheet. Retrieved January 15, 2026, from https://www.who.int/news-room/fact-sheets/detail/breast-cancer
- World Health Organization (WHO). (n.d.). Lung cancer – Fact sheet. Retrieved January 15, 2026, from https://www.who.int/news-room/fact-sheets/detail/lung-cancer
- World Cancer Research Fund International. (n.d.). Stomach cancer statistics. Retrieved January 15, 2026, from https://www.wcrf.org/preventing-cancer/cancer-statistics/stomach-cancer-statistics/


