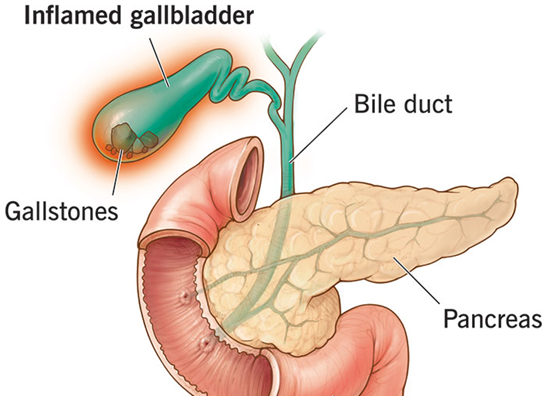
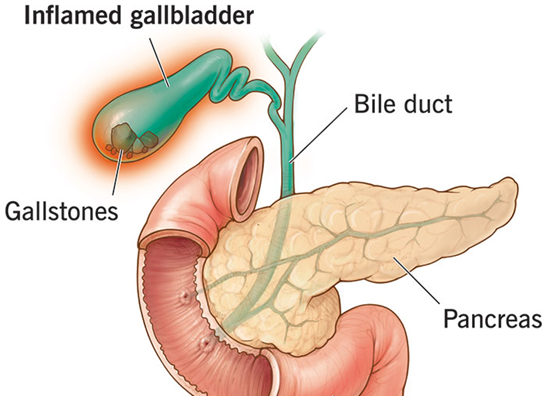
Cholelithiasis/Gall stones
Cholelithiasis refers to the presence of gallstones in the gallbladder, which can range in size from as small as a grain of sand to as large as a golf ball. These stones can be single or multiple and may pass into other parts of the biliary tract, including the cystic duct and common bile duct, a condition known as choledocholithiasis. Gallstones may cause blockages, leading to symptoms such as pain, nausea, and digestive issues.
Prevalence
Gallstones, a leading cause of cholecystitis, are present in approximately 10–15% of the general population, with variations across countries. Between 20% and 40% of individuals with gallstones may develop complications such as acute cholecystitis. (WJES, 2020)
Types
There are three types of gall stone
- Cholesterol stones: Yellow stones primarily made of cholesterol; common in cases of excess cholesterol or bile stasis.
- Pigment stones: Dark stones composed of bilirubin and calcium salts; associated with chronic hemolysis or liver diseases.
- Mixed stones: A combination of cholesterol, bile pigments, and calcium salts; often linked to recurrent gallbladder inflammation
Causes
- Cholesterol supersaturation: Most gallstones form due to an excess of cholesterol in bile.
- Reduction in bile salts: Insufficient bile salts to dissolve cholesterol leads to stone formation.
- Disturbed cholesterol metabolism: Imbalance in cholesterol processing contributes to gallstone development.
- Obstruction of bile flow: Blocked bile flow from the gallbladder promotes stone formation.
- Gallbladder damage or infection: Inflammation or infection causes bile stasis, increasing the risk of gallstones.
Predisposing factors
- Family History – A genetic predisposition to gallstone formation is common in some families.
- Dietary pattern – Diets rich in cholesterol, fats, and refined carbohydrates but low in fiber can increase the risk of gallstone formation.
- Obesity – Excess body weight is associated with higher cholesterol levels in bile, contributing to gallstone formation.
- Oral contraceptives – Hormonal changes induced by oral contraceptives may alter bile composition and increase gallstone risk.
- Lipid-lowering drugs – Certain drugs that lower cholesterol levels may inadvertently lead to gallstone formation by increasing cholesterol excretion into bile.
- Certain diseases:
- Crohn’s disease – Chronic inflammation of the gastrointestinal tract can interfere with bile salt reabsorption, promoting gallstone formation.
- Cirrhosis – Liver dysfunction may impair bile production and lead to gallstones.
- Biliary infections – Infections in the biliary system can contribute to bile stasis and stone formation.
The 4 F’s of gallstone risk factors is a mnemonic used to identify key predisposing factors for gallstone formation:
- Female – Women are at higher risk due to hormonal factors, especially during pregnancy or with the use of oral contraceptives.
- Forty – Gallstones are more common in individuals over 40 years of age.
- Fertile – Increased risk is associated with pregnancy and multiple childbirths due to hormonal changes that affect bile composition.
- Fat – Obesity or being overweight is a significant risk factor as it increases cholesterol levels in bile.
Pathophysiology
Cholelithiasis, or the formation of gallstones, occurs when there is an imbalance in the substances that make up bile, leading to the formation of stones in the gallbladder. The pathophysiology can be understood based on the types of gallstones: cholesterol stones and pigment stones.
1. Cholesterol stones
- Bile composition imbalance: Bile, produced by the liver, is essential for the digestion and absorption of fats. It contains cholesterol, bile salts, and phospholipids. Normally, cholesterol is dissolved in bile. However, if there is too much cholesterol in bile (due to factors like obesity, high-fat diets, or liver disease), it becomes supersaturated and can crystallize.
- Crystallization and stone formation: These cholesterol crystals can form within the gallbladder, and over time, they combine to form larger stones. The stones are often yellow-green in color and can range in size from small grains to large stones.
- Impaired gallbladder motility: If the gallbladder does not empty properly (due to factors like obesity, pregnancy, or certain medications), bile stasis can occur. The prolonged stasis increases the chances of cholesterol crystallization.
- Risk factors: High cholesterol, obesity, pregnancy, diabetes, and certain medications (such as oral contraceptives or hormone replacement therapy) are risk factors for cholesterol stone formation.
2. Pigment stones
- Excess Bilirubin: Pigment stones are primarily composed of bilirubin, a byproduct of red blood cell breakdown. When there is excess bilirubin in the bile, either due to increased red blood cell turnover (as in hemolysis) or liver dysfunction (such as cirrhosis), it can form calcium salts, leading to the formation of stones.
3. Gallbladder dysmotility and bile stasis
- Impaired gallbladder emptying: Inadequate emptying of the gallbladder leads to bile stasis, which contributes to the formation of gallstones. This can occur due to pregnancy, obesity, fasting, or disease-related factors that affect gallbladder motility.
- Bile viscosity: When bile becomes more concentrated due to poor motility or dehydration, it increases the risk of forming crystals and stones.
Signs and symptoms
- May not produce noticeable symptoms initially.
- Discomfort or pain in the upper abdomen.
- Pain localized to the right side of the upper abdomen.
- Pain may extend to the back or right shoulder.
- Symptoms often occur after consuming fatty meals, typically worsening at night.
- Nausea and Vomiting common accompanying symptoms.
- Vitamin deficiency possible due to malabsorption of fat-soluble vitamins (A, D, E, K).
- Other symptoms:
- Jaundice (yellowing of skin and eyes)
- Clay-colored stools (due to obstruction of bile flow).
Diagnostic Evaluation
- Blood Tests
- Serum Bilirubin Test: Detects liver dysfunction or bile duct blockages.
- Liver Function Test (LFT): Measures ALT, AST, ALP, and albumin to assess liver function.
- Complete Blood Count (CBC): Identifies anemia, infection, or disorders affecting liver health.
- Prothrombin Time (PT): Evaluates blood clotting; prolonged PT may indicate liver disease.
2. Ultrasound (USG) abdomen: Detects gallstones (90% accuracy) and other abnormalities like tumors or inflammation.
3. Cholecystography: X-ray imaging to visualize gallstones, inflammation, or bile duct issues.
4. Endoscopic Retrograde Cholangiopancreatography (ERCP): Combines endoscopy and X-ray to diagnose and treat bile duct, gallbladder, or pancreatic conditions, including gallstone removal and blockages.
5. Magnetic Resonance Cholangiopancreatography (MRCP): Non-invasive MRI providing detailed images of biliary and pancreatic ducts to detect stones, strictures, or tumors.
6. Percutaneous Transhepatic Cholangiography (PTC): Uses contrast dye injected through the liver to identify biliary blockages or abnormalities, useful when ERCP is not feasible.
Medical Management
- Oral ursodeoxycholic acid and chenodeoxycholic acid: These are cholesterol-dissolving agents used to dissolve small cholesterol gallstones in patients who are not suitable for surgery. Treatment is long-term and works best for non-calcified stones.
- Antibiotics: Prescribed in cases where there is associated infection, such as cholecystitis or cholangitis. Common antibiotics include ceftriaxone or metronidazole.
- Non-surgical gallstone removal (Lithotripsy): Extracorporeal shock wave lithotripsy (ESWL) uses sound waves to break gallstones into smaller fragments that can be passed through the bile duct. Typically reserved for patients unfit for surgery.
- Supportive measures for mild attacks: Bed rest is encouraged during mild attacks to reduce physical strain. Intravenous fluids maintain hydration and correct electrolyte imbalances, especially in cases of vomiting. Nasogastric suction is used to relieve abdominal distension and prevent aspiration in severe cases.
- Dietary modifications: A low-fat diet is recommended to reduce biliary colic episodes and avoid stimulating the gallbladder.
- Vitamin K supplementation: Administered if prolonged obstruction or bile duct involvement leads to a deficiency in fat-soluble vitamins, affecting blood clotting.
Surgical Management
- Cholecystectomy
- Open Cholecystectomy: Performed through an abdominal incision; used for complicated or severe cases.
- Laparoscopic Cholecystectomy: A minimally invasive technique preferred for most patients due to faster recovery, minimal scarring, and reduced pain.
- Choledochotomy
- A surgical procedure involving the opening of the common bile duct to remove stones or relieve obstruction. Often used in conjunction with ERCP (Endoscopic Retrograde Cholangiopancreatography).
Nursing diagnosis
- Acute pain related to surgical incision and ambulation as evidenced by patient verbalizing pain, guarding, or difficulty moving.
- Discomfort related to the presence of nasogastric (NG) tube as evidenced by patient verbalizing throat irritation, discomfort, or difficulty swallowing.
- Impaired physical mobility related to post-operative pain and incisional discomfort as evidenced by limited range of motion or difficulty ambulating.
- Imbalanced nutrition less than body requirements related to anorexia and decreased food intake as evidenced by reduced appetite, weight loss, or insufficient nutritional intake.
- Deficient knowledge related to post-operative care, dietary restrictions, and follow-up treatments as evidenced by patient asking for clarification and expressing uncertainty about home care instructions.
- Risk for infection related to impaired wound healing and self-care deficit as evidenced by surgical incision, presence of drainage, and limited ability to perform self-care activities.
- Risk for deficient fluid volume related to decreased fluid intake and increased fluid loss during surgery as evidenced by dry mucous membranes, reduced urine output, or patient verbalizing decreased thirst.
Nursing interventions ( Cholelithiasis/Choledocholithiasis)
- Assess the general condition: Evaluate the patient’s overall physical and emotional state to establish a baseline and identify any immediate needs.
- Monitor Vital Signs and record: Regularly check temperature, blood pressure, pulse, and respiration to detect early signs of complications.
- Provide a comfortable position: Ensure the patient is positioned to alleviate pain and improve breathing, such as semi-Fowler’s position.
- Administer sedatives and analgesics for pain: Provide prescribed medications to manage pain and enhance comfort.
- Encourage verbalization of fears and emotions: Allow the patient to express their feelings to reduce emotional distress and build trust.
- Explain every procedure to reduce anxiety: Provide clear and concise explanations about procedures to help the patient feel informed and calm.
- Check T-Tube for kinks and attachment: Inspect the T-tube to ensure proper drainage and prevent complications like bile leakage or infection.
- Measure and record T-Tube drainage daily: Document the amount and characteristics of drainage to monitor recovery progress.
- Provide comfort measures; Maintain personal hygiene, encourage ambulation, and ensure a clean and safe environment to promote comfort.
- Monitor nutritional status: Assess the patient’s diet and encourage a low-fat diet to reduce strain on the biliary system.
- Provide education: Educate the patient on proper dietary habits, adequate rest, and maintaining a healthy sleep schedule.
- Encourage deep breathing and coughing exercises: Promote exercises to prevent respiratory complications and improve lung expansion.
- Engage in diversion therapy: Introduce activities to divert attention from pain and anxiety, such as relaxation techniques or light reading.
- Discharge teaching; Provide guidance on wound care, prescribed medications, dietary modifications, and the importance of follow-ups to ensure proper recovery.
Sources: Waugh, A., & Grant, A. (2012). Ross and Wilson Anatomy and Physiology in Health and Illness (11th ed.). Reed Elsevier India Private Limited.
For additional link click below:
https://ajmanavta.com/laparoscopic-surgery
https://wjes.biomedcentral.com/articles/10.1186/s13017-020-00336-x?utm
https://my.clevelandclinic.org/health/diseases/15265-gallbladder-swelling–inflammation-cholecystitis
https://www.mayoclinic.org/diseases-conditions/gallstones/symptoms-causes/syc-20354214rgery



